Author: Shayne Polley (PGY3)
Public Health Indian Hospital Rotation
Tséhootsooí Medical Center Fort Defiance, Arizona – on the Navajo Reservation
Our Emergency Medicine Residency Program at ACMC is unique for several reasons – we rotate one-to-one attending-with-resident while on-shift in the ED; we rotate only at Advocate Christ Hospital, which allows us to foster relationships with off-service residents and consultants; and we have three full one-month electives to dedicate towards our individual interests. Often, residents will choose to pursue in-house rotations within our program, such as Resuscitation, Pharmacotherapy or Critical Care electives. However, these months also offer the opportunity to explore niches within Emergency Medicine off-site, with alternative rotations available such as a rural EM experience in Idaho or Alaska (which I have upcoming) or a Global Health elective abroad (also planning). If there is a personal area of interest in which an elective is not yet established, our program also supports us in pursuing a new rotation or elective experience.
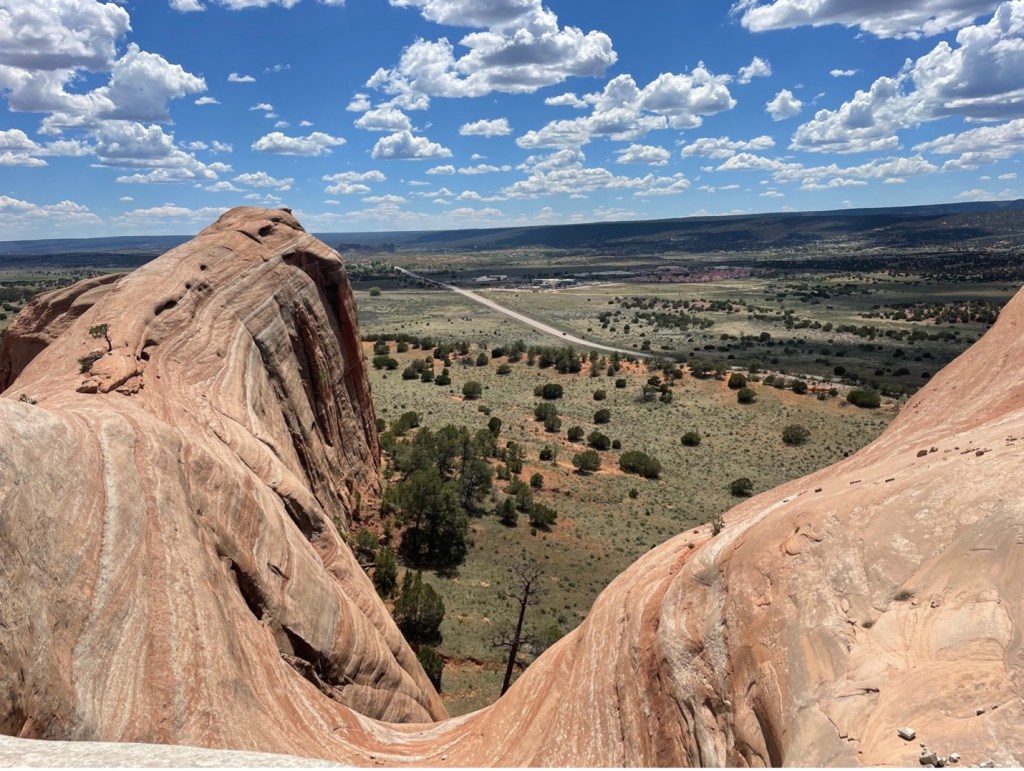
I had the privilege of pioneering one such new rotation, a Public Health rotation on a Navajo Reservation in Arizona. I completed this Public Health Indian Hospital Rotation at Tséhootsooí Medical Center in Fort Defiance, Arizona, at the end of my second year of residency – and it was a truly phenomenal experience, from start to finish. This hospital site is located in Northeast Arizona on the Navajo Reservation, along the border of Arizona and New Mexico. The hospital itself is a limited-access remote hospital with an 11-bed ER – dramatically different than our home institution, a large level 1 Trauma, tertiary care hospital with all the bells and whistles (and in-house consultants).

This proved to be an incredibly gratifying and meaningful experience, and not only in furthering my personal interests in Global and Public health by providing care to a traditionally underserved population. It also to gave me the opportunity to practice Emergency Medicine in an environment starkly different from my home institution, with dramatically different resources.

Tséhootsooí Medical Center is a 56-inpatient-bed hospital with a small, limited ICU, and very few subspecialists. During the rotation, I worked 10-hour shifts one-on-one with ED attendings in the 11-bed ER. The ED has a CT scanner, and on weekdays during business hours, does have a formal ultrasonographer as well. It has some specialties in-house including general surgery and pediatrics. However, the hospital lacks many subspecialists such as cardiology GI and neurology, with whom I am accustomed to speaking with regularly on-shift at ACMC, let alone others such as neurosurgery, hematology or infectious disease. It certainly doesn’t have an MRI, or other inpatient capabilities such as stress testing or endoscopy.

Throughout my shifts, I saw a great variety of chief complaints, some of which I was able to manage similarly to how I might in my own institution. For example, with abdominal pain in a febrile elderly patient, I readily ordered my sepsis evaluation and CT scan; decreased po intake with vomiting in a well-appearing child, I gave the antiemetic and po challenged. However, I found a dramatic difference in management of critical patients, and those requiring further inpatient work ups with subspecialists. Chest pain evaluations with positive troponins or concerning ACS stories required transfer via helicopter to hospitals that could have them further evaluated and managed by cardiology. A STEMI would require thrombolytics, stabilization and transport to an accepting hospital with a cardiologist waiting in the cath lab. The acute upper GI bleed actively vomiting blood would not quickly get whisked away to the GI suite, but rather would require stabilization then transport by helicopter as well. The altered pediatric patient with concern for possible nonaccidental trauma found to have an acute SDH, required intubation, discussion with an accepting hospital’s pediatric neurosurgery team, and transport as well. I became very familiar with coordinating transport and speaking with accepting physicians at several hospitals throughout the Desert Southwest. I ordered a lot of helicopters.

Some of the complaints were also more unique to this underserved patient population. In planning for transfer, I had to recognize that often these patients were being moved via air 1-2 hours from their families; a three-plus-hour drive often not feasible for parents or loved ones to travel. On this “dry” reservation, there is also a significant population of alcohol use disorder, with all the comorbidities associated with this. There is also a notable incidence of toxic alcohol ingestion, with patients presenting after ingesting ethanol or hand sanitizer, a cheaper alternative to the less accessible alcohol, until they become severely ill. Regionally, I also had new differentials on the forefront such as Hantavirus, something I would not expect to see in the Midwest but was regularly screened for in patients on the reservation in the desert.

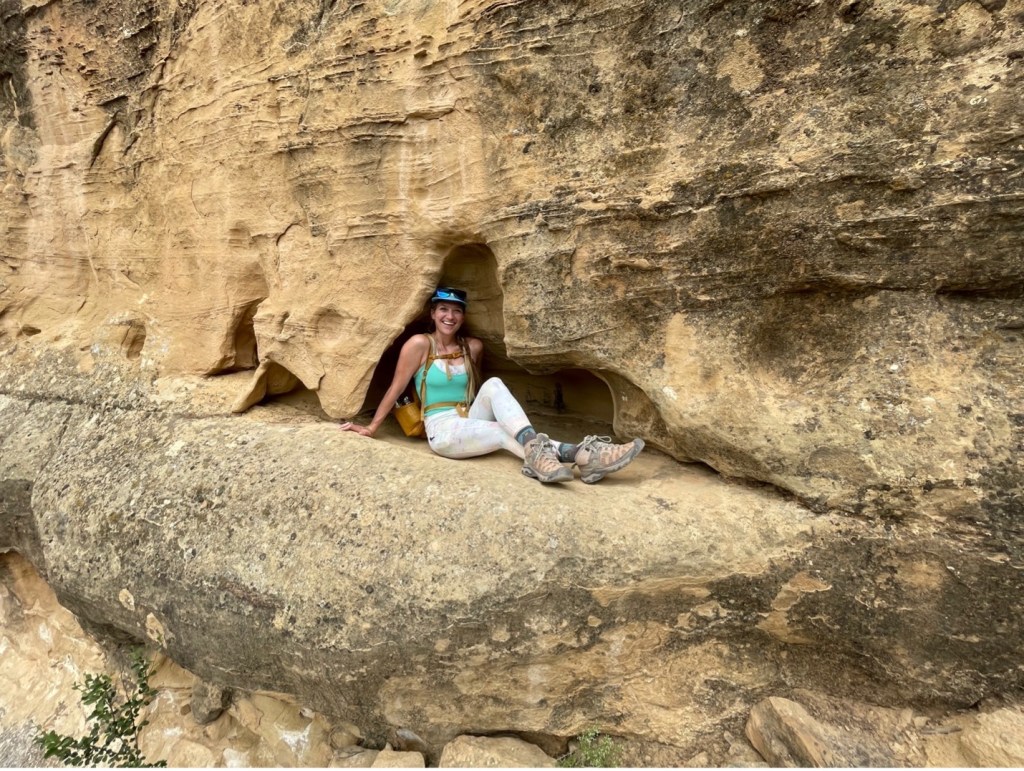
Outside of the hospital, this rotation offered a great deal of adventure as well. I lived on the Navajo Reservation right next to the hospital and could walk the 3-minute commute to work (with little prairie dogs chirping along the way). There was a local gym which I could join for a nominal fee. Just beyond the hospital, there were some beautiful desert hikes to enjoy during down time. During one of my hikes on the local BellyButton trail just next to the hospital, a friend and I found a poor stray pup that had become trapped in the “belly button,” within the cliff; we spent the next hour working to rescue the pup – with success!



This month also had plenty of downtime from shifts away from work, where I could plan longer adventures. Regionally, it has a great deal of National Parks within a reasonable drive – such as the Petrified Forest, Mesa Verde, the Grand Canyon, and just a bit further Zion, Bryce, Arches and others. I happened to hit eight national parks hiking, camping and exploring during my stretches of time off – and it was one of the best months of my life!




I’ll say it again – this was one of the gratifying and exciting experiences of my life – for the medicine I got to practice, the people I cared for, and the adventures I had. And, I mentioned at the start of this post, this is only one of three electives I’ve had the privilege to enjoy. I have scheduled an upcoming Remote EM Elective for one month in Alaska; and at the end of my third year, I will be coordinating a Global Health Elective somewhere in Central or South America. The support of my residency in pursuing these interests, is only one of the many reasons I am so proud to be an EM residency training at Advocate Christ.